 Innovative methods for managing pain after cosmetic surgery are being combined to enhance patient comfort during procedures. These approaches include:
Innovative methods for managing pain after cosmetic surgery are being combined to enhance patient comfort during procedures. These approaches include:

- Topical Anesthetics: Prior to skin injection, surface anesthetics like Ethyl Chloride are used. Ethyl Chloride quickly freezes the skin, overwhelming pain-transmitting nerves with cold sensation, reducing pain recognition. Local anesthetics like benzocaine, lidocaine, and others are now formulated as creams or gels to induce numbness before treatment. These are applied 20-30 minutes prior, often covered with plastic wrap for better absorption. They are especially popular for cosmetic laser and injectable procedures.
- Regional Anesthetics: For sensitive areas like lips, specific sensory nerves transmitting pain are numbed using local anesthetics. This ensures painless procedures like lip augmentation with fillers. Dr. Laverson uses topical anesthetic on the skin, then carefully numbs the specific nerves that supply sensation to your lips. This allows completely pain free lip enhancement. Filler must be placed well within the substance of the lips, and topical (surface) anesthetic doesn’t penetrate deeply enough to sufficiently numb your lips without addition of a regional anesthetic to block pain impulses.
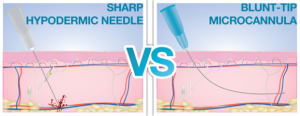
- Cannulas Instead of Needles: Blunt-tipped sterile cannulas are now used for injectables, minimizing trauma to surrounding tissues and reducing the risk of nerve or blood vessel injury. These cannulas offer the added benefit of avoiding nerve or blood vessel injury. Sharp needles more easily cut small nerves and vessels beneath the skin, leading to bruising and other side effects. Blunt tipped cannulas, when carefully used, are more likely to push aside these structures, allowing injection to proceed with less trauma to surrounding tissues.
- Long-Acting Local Anesthetics: Exparel®, a long-acting local anesthetic, is injected before surgical closure. It slowly releases bupivacaine over a few days, significantly reducing post-surgical pain and lessening the need for narcotic analgesics. Exparel® can be distributed within your tissues before surgical closure. While not totally eliminating post-surgical pain, your discomfort may be reduced to a much more tolerable level. Use of Exparel® may diminish your dependence on narcotic analgesics such as morphine, oxycodone, meperidine, hydromorphone, and hydrocodone, all of which have undesirable side effects.
- Nausea Prevention: Nausea prevention is crucial as many potent pain medications cause nausea. Anti-nausea medications like ondansetron, scopolamine patches, and others complement pain management by narcotics, enhancing the overall surgical experience. First off, if you are nauseated after rhinoplasty, breast implants, or tummy tuck, you’re unable to hold down pain medicine. You’re not only nauseated, but in pain, a difficult combination. Second, if you’re vomiting after nose, face, breast, or liposuction surgery, the entire experience of aesthetic enhancement becomes tainted with bad memories. We plastic surgeons want to prevent nausea and vomiting as much as possible, knowing that if you are miserable, you’re less likely to come back for more. The introduction of anti-nausea medications such as ondansetron (Zofran®), aprepitant (Emend®), scopolamine skin patch (Transderm SCOP®), and alvimopan (Entereg®) combined with traditional anti-nausea treatments droperidol, metoclopramide, and others offer much improved pain control by narcotics and a better surgical experience.
- Non-Narcotic Analgesics: Intravenous acetaminophen, ketorolac in recovery, and extended-release tramadol at home provide pain relief with fewer side effects than traditional narcotics. Muscle relaxers like Carisoprodol (Soma®) are also helpful.

 Book Now
Book Now











